Lumbar spine chondropathy is a chronic disease that develops due to the process of degenerative disc dystrophy. This disease is common and affects most people between 25 and 40 years old.
According to statistics, the second adult has experienced back pain at least once in his life, and in 95% of the cases, this is caused by spinal chondrosis.
Patients with severe lumbar osteochondrosis, persistent pain and other manifestations are considered temporary disability. If their condition does not improve within four months, it is decided to establish a group of persons with disabilities.
Causes and risk factors
The factors leading to the development of lumbar spine chondropathy are:
- Abnormal spine structure;
- Lumbar spondylosis-congenital pathology of the spine, which is characterized by the separation of the first vertebra from the ac bone and transforming into the sixth (additional) lumbar vertebra; Sa ossification is a congenital pathology in which the fifth lumbar vertebrae fused with the bone. Asymmetric arrangement of intervertebral joint space;
- Pathological stenosis of the spinal canal;
- reflects spontaneous pain (body and muscle);
- Obesity;
- Sedentary lifestyle;
- Exposure to vibration for a long time;
- The physical pressure of the system;
- Smoking.
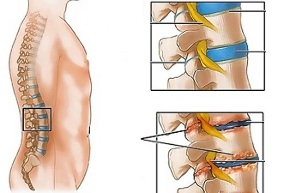
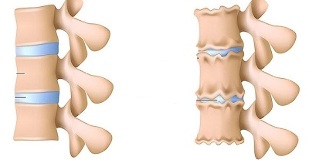
The combination of unfavorable static dynamic load and one or more risk factors can cause changes in the physiological characteristics of the nucleus pulposus of the fibrous disc, thereby damping shock and providing spine mobility. The process is based on the depolymerization of polysaccharides, which results in the loss of water in the gelatinous nuclear tissue. As a result, the nucleus pulposus and the fiber disc lose their elasticity. Further mechanical stress will cause the fiber ring to protrude and lose its elasticity. This phenomenon is called protrusion. A crack appears in the fibrous nucleus, through which fragments of the nucleus pulposus fall off (prolapse, herniated disc).
Over time, the long-term compression of nerve roots innervating certain organs in the abdominal cavity will cause their function to deteriorate.
The instability of the spine segments is accompanied by the reactivity of the adjacent vertebrae and intervertebral joints, as well as the development of spondyloarthropathy. For example, in the context of physical activity, significant muscle contraction can cause the vertebral body to shift, and with the development of neurological syndrome, the nerve root can become stuck.
The form of the disease
Depending on the structure involved in the pathological process, lumbar osteochondrosis can be clinically manifested by the following syndromes:
- Reflex-low back pain, low back pain, low back pain; developed against the background of excessive back muscle reflex;
- Compression (spinal cord, blood vessel, nerve root)-Compression (compression) of the spinal cord, blood vessel or nerve root causes its development. Examples are lumbar radiculitis and radiculopathy.
Symptoms of lumbar osteochondrosis
In lumbar osteochondrosis, the symptoms are determined by the structures involved in the pathological process.
Low back pain occurs under the influence of hypothermia or physical stress, sometimes without obvious cause. The pain is sudden and shooting. Sneezing, coughing, turning around, exercising, sitting, standing, and walking all exacerbate this condition. In the supine position, the pain is significantly reduced. Retain sensitivity and reflex, reduce the range of motion of the lumbar spine.
Palpation observation:
- Sore waist;
- Paravertebral muscle spasm;
- Lumbar lordosis becomes flat, and in many cases scoliosis.
Negative nerve root tension syndrome for low back pain. When raising the straight leg, the patient will notice increased pain in the waist area, but no pain in the lower limb straightening.
Usually, lumbar osteochondrosis causes recurrence of painful episodes, each of which becomes more intense and continuous.
Healthcare
Vasomotor disease is a characteristic of low back pain:
- Changes in skin temperature and color of lower limbs;
- Feeling cold or hot;
- Blood circulation disorders.
The development of lumbar spine compression syndrome is clinically manifested as the following symptoms:
- Skin hyperalgesia;
- The pain of shooting;
- Reduce or completely lose deep reflections;
- Peripheral paralysis.
When suffering from compression syndrome, bending the torso, sneezing and coughing will exacerbate the pain.
Diagnosis
In the blood test on the background of lumbar osteochondrosis:
- Decreased calcium concentration;
- Increased ESR;
- Increase alkaline phosphatase levels.
In the diagnosis of lumbar osteochondrosis, X-ray examination of the spine is very important.
Over time, the long-term compression of nerve roots innervating certain organs in the abdominal cavity will cause their function to deteriorate.
The X-ray signs that can confirm the diagnosis are:
- Change the configuration of the affected segment;
- Pseudo spondylolisthesis (displacement of adjacent vertebral bodies);
- Deformation of the closed plate; Flatten the intervertebral disc;
- Unequal disc heights (symptoms of spacers) are related to asymmetric muscle tension.
can also be used in the diagnosis of lumbar osteochondrosis:
- Myelography, computer or magnetic resonance imaging-essential for the development of persistent symptoms, neurological deficits;
- Scintigraphy (to study the accumulation of phosphorus in the skeletal system, marked as tech-99)-If a tumor or infection process is suspected, spinal cord injury.
Differential diagnosis of lumbar osteochondrosis for the following diseases:
- Spondylolisthesis;
- Dysentery spondylosis;
- Ankylosing spondylitis (ankylosing spondylitis);
- Infection process (disc inflammation, spinal osteomyelitis);
- Tumor formation process (primary spinal tumor or its metastatic disease);
- Rheumatoid Arthritis;
- Deformable osteoarthritis of the hip joint;
- Reflects pain (diseases of internal organs and large blood vessels).
Treatment of lumbar osteochondrosis
For lumbar osteochondrosis, the following treatment strategies are usually followed:
- Bed rest for 2-3 days;
- Traction the affected spine segment;
- Strengthen the muscles of the back and abdomen (form a so-called muscle corset);
- Effect on pathological myofascial and myotonia process.
Low back pain occurs under the influence of hypothermia or physical stress, sometimes for no obvious reason.
In most cases, conservative treatment of lumbar osteochondrosis includes the following measures:
- The infiltration anesthesia of the muscle with local anesthetic solution;
- Take non-steroidal anti-inflammatory drugs;
- Take desensitizer;
- Vitamin therapy;
- Take sedatives and antidepressants;
- Manual therapy, massage;
- Physiotherapy practice;
- Acupuncture; Relax after isometric.
The absolute indications for surgical treatment of lumbar osteochondrosis are:
- Acute or subacute spinal cord compression;
- The development of cauda equina syndrome is characterized by pelvic organ dysfunction, sensory and movement disorders.
Therapeutic exercise for lumbar osteochondrosis
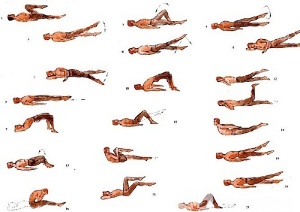
Physical therapy plays an important role in the comprehensive treatment of lumbar osteochondrosis. Regular exercise can normalize the muscle tension of the paraspinal muscles and improve the metabolic processes in the tissues affected by the pathological process. In addition, it can also form a developed muscle corset to support the spine in the correct position, thereby reducing unnecessary spineThe static load.
In order to maximize the effect of gymnastics for lumbar osteochondrosis, the following principles should be followed:
- The regularity of the class;
- The intensity of physical activity gradually increases;
- Avoid fatigue during class.
Physiotherapy should be carried out under the guidance of an experienced coach who will choose the most effective exercise for a specific patient and control the correctness of its implementation.
According to statistics, the second adult has experienced back pain at least once in his life, and in 95% of cases, this is caused by spinal chondropathy.
In addition to class with the instructor, you should also do a set of morning exercises every day, which includes special exercises for lumbar spine chondrosis.
- Relaxation and contraction of abdominal muscles.The starting position is to stand, with your feet shoulder-width apart and your arms lowered to your body. Hold your breath and relax the muscles of the front wall of your abdomen. During the exhalation, diarrhea as much as possible, straining the abdominal muscles. Exercise should be repeated until mild fatigue occurs.
- Head movement with curvature of the spine.The starting position is on your knees. Put your arms straight on the floor and straight back. Slowly raise your head and bend back. Stay in this position for a few seconds, then return to the starting position smoothly. Repeat at least 10-12 times.
- "Pendulum".The starting position is supine, arms along the body, legs bent at right angles at the knees and hip joints. Rotate your legs to the left and right in a swing-like pose, trying to reach the ground. In this case, the shoulder blade cannot be torn off the floor.
- Ship.Lie on your back in the starting position with your arms extended forward. Tear off the upper body and legs from the floor and bend back. Hold this position for 5-6 seconds, then slowly return to the starting position. Run 10 times.
Potential consequences and complications
The main complications of lumbar osteochondrosis are:
- The formation of intervertebral disc hernia;
- Vegetative vascular dystonia;
- Lumbar spondylolysis, spondylolisthesis;
- Osteophytes;
- Spondyloarthropathy; Spinal stenosis results in compression of the spinal cord, which may lead to permanent disability and reduced quality of life.
Over time, the long-term compression of nerve roots innervating certain organs in the abdominal cavity will cause their function to deteriorate. As a result, the patient suffers from bowel dysfunction (constipation, diarrhea, flatulence) and pelvic organs (urinary system disease, erectile dysfunction, cold, infertility).
Forecast
The pain syndrome of lumbar osteochondrosis appears in the form of relief and aggravation. The low back pain lasted for 10-15 days, after which the patient's condition improved and the pain relieved. Related secondary diseases can prevent a good prognosis. Usually, lumbar osteochondrosis has recurring episodes of pain, each of which becomes more severe and continuous.
Physical therapy plays an important role in the comprehensive treatment of lumbar osteochondrosis.
Patients with severe lumbar osteochondrosis, persistent pain and other manifestations are considered temporary disability. If their condition does not improve within four months, it is decided to establish a group of persons with disabilities.
Prevention
Preventing the development of osteochondrosis of the spine includes the following measures:
- Quit smoking;
- Weight normalization;
- Improve general physical condition, active lifestyle;
- Avoid provocative conditions (lifting weights, sudden movements, turning, bending).












































